Our Story

The Durham Dales Health Federation was established in 2014.
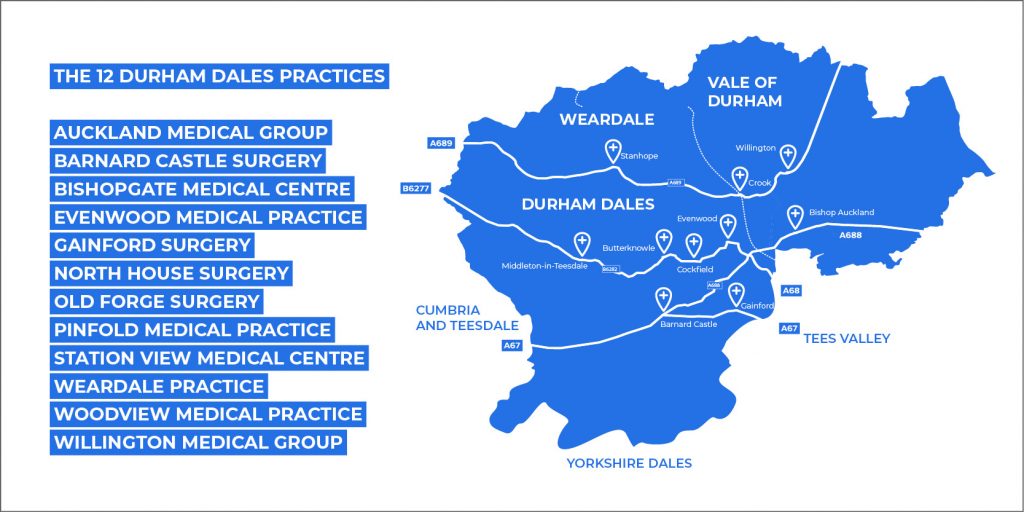
A group of 12 GP practices across Durham Dales got together, looking for a solution to help them provide the care patients needed, share resources and ideas, and be prepared for the challenges the NHS would face in the future.
The answer they came up with was a formal collaboration between the dozen practices: the Durham Dales Health Federation
DDHF’s founding principal is to work together to provide high-quality, cost effective primary healthcare services.
That means providing a range of services that all GP practices in the area can use to help look after patients.
We are a not-for-profit organisation, and part of the NHS.
In 2014, the NHS launched it’s 5 Year Forward View. This was a plan to address the building pressures on NHS services and to respond to the changing needs of patients.
While the NHS had improved in the previous 15 years with waiting times down and patient satisfaction on the rise, the quality of care varied from one area to another and preventable illnesses were still widespread.A ‘one size fits all’ model wouldn’t meet the differing needs of each community, so there was a need for new ideas and local leadership. The NHS plan made it easier for groups of GP practices to work together as networks or federations.
It was against this backdrop that the 12 Durham Dales GP practices met to discuss their options and decide what they should do.
Fledgling federations had appeared across the region, and joining an existing grouping was a distinct option.
After careful and detailed discussion about the specific needs of patients, a strong history of cooperation and a distinct collective identity across the Dales, it was decided to go it alone.
The Durham Dales Health Federation was born, with a GP or manager from each of the 12 member Practices forming our Board.
Our first piece of contracted work was to deliver a service that ensured the most vulnerable 2% of adults in the area were looked after.
Typically frail and elderly people with advanced or very specific needs, it was decided a standalone service would be best placed to serve their needs, freeing up considerable amounts of GP practices’ time.
All 12 practices pooled funding to support what has become known as VAWAS - our Vulnerable Adults Wrap Around Service.
This first service started with just one nurse building to a team of 4 by the start of 2016.
The team worked with vulnerable adults - primarily aged over 75 - to create personalised care plans.
This proactive approach took a holistic look at patient care, with the aim of reducing avoidable hospital admissions, and keeping people safe and well in their homes.
In the years that have followed, the service has developed into a nurse-led, multidisciplinary Community Wellness Team that has created over 2,500 individual patient plans, reducing admissions by 20%.
It has also led the way in creating new teams and new services to fulfil unmet needs that have been identified along the way.A case in point is the development of Health Care Coordinators - a team of non-clinical staff who would care for the social needs of patients, allowing the medical team to concentrate solely on clinical issues. A case study on the evolution of Health Care Coordinators can be found here.
Integrated Diabetes Service was another that we built from the ground up.
We work alongside a specialist Diabetic nurse to up-skill Practice Nurses across Durham Dales. In turn, Practice Nurses would then be able to lead clinics for people with diabetes, creating individual treatment plans which improved patients’ knowledge and their ability to better manage their health. Collectively, our Integrated Diabetes Services has produced some of the best outcomes for diabetic patients. Further information can be found in our Services section.In 2017 we launched Extended Primary Care Access (EPCA) - a way to support our member practices to be able to offer more same day appointments, and more outside of normal hours.
Part of this service was encouraging patients to either call their GP practice or 111 in advance - either to be booked in for an appointment, or to be directed towards other options or self-care advice. This meant clearer paths for people to quickly get to the right service for their needs. The service initially ran from various practice hubs throughout the 3x Primary Care Network areas however to make this more accessible for patients this is now centralised for Durham Dales in Bishop Auckland General Hospital.
In 2021 DDHF was successful in being awarded a contract to pilot a similar service in University Hospital of North Durham with the addition of Care Navigation directly from Accident & Emergency as well as via 111. This pilot has continued and is working extremely well with continued contract extensions.
Both services are now known as Same Day Urgent Care.
With a GP and Advanced Nurse Practitioners based in hubs, we’ve made it easier for patients to get seen sooner, taking significant pressure off urgent care services.
The cost to the NHS of a patient being seen by our EPCA service is only 60% the cost of them being seen in an urgent care unit. As well as quick, appropriate care to patients, we’re providing value for money for the health service.
Our business model is all about efficiency.
While we hold a number of different contracts for different services, we treat them as one collective in the way we recruit, develop and deploy our staff.
Our logic is to have a smaller number of staff working more hours across a number of contracts, rather than more staff working short hours wholly within one particular service with the added variety and mix of skills for staff if cross cover needed between contracts.Staff recruitment becomes easier, as we can offer more shifts and stability. Our training and development budgets cover fewer people, so can take each one of them further. We offer many benefits for working with us these are shown on our Recruitment pages
Most importantly of all, it means patients who come across our staff in different settings experience a consistent, high level of care.
This combination of efficiency and continuity allows us to deliver high-quality services whilst also funding our management infrastructure.
We’re unlike other health federations in that our management team brings a range of different skills and experiences from both inside and outside of the NHS. That mix of expertise - from business and the commercial sector to charities and the military - adds a unique perspective to how we operate.We explore, innovate and develop new ideas that bring benefits to patients and support our member practices with coordination, project management and specialist HR and financial advice.
Through our business intelligence and development, we analyse and monitor trends helping to identify potential issues, and proactively seek solutions.
From a strong evidence base, we can focus on delivering better outcomes for patients, and better value for money for commissioners.
We don’t just work to make our existing services better.
We work to identify new systems, processes and services to tackle unmet needs.
Case studies on some of our most interesting, impactful and innovative developments can be found below.
In addition to our continuous improvements on delivering services on our existing contracts we also work to identify new opportunities and new contracts for expanding the organisation further within the locality. Contracts over the past year have allowed us to showcase our staff and services as well as our ability to quickly mobilise our teams and services along with the extensions to our existing contracts ensures we are always an approachable organisation for new innovations and new services. Examples of some of these contracts are:- FeNO pilot - In 2021 DDHF were successful in being awarded a pilot contract in conjunction with Wessex Academic Health Science Network (AHSN) for Fractional exhaled Nitric Oxide (FeNO) which is an objective test providing an indication of the level of eosinophilic inflammation in the lungs. The pilot was used over the year as part of the diagnostic pathway for new asthma cases as well as ongoing reviews of treatment for existing asthma patients. The pilot involved 2 machines, one situated in our Same Day Urgent Care hub at Bishop Auckland and one as a roving unit booked out to the 12 practices within Durham Dales. The duration was 1 year completing in July 2022 with a full evaluation provided.
https://www.niox.com/en-gb/digital-platform/ahsn-feno-mission/ https://healthinnovationwessex.org.uk/projects/603/feno-pathway-transformation-report-library
- During the pilot
- 50 staff were training in using the machines
- 129 patients were booked in to access the testing
- 96 patients were testing for first time asthma
- 30 patients received an asthma diagnosis as a result of the tests
- During the pilot
- Flu Vaccinations for 2-3 year old - In September 2022 DDHF were asked by the Integrated Care Board (ICB) to provide vaccinations for 2-3 year olds throughout County Durham due to the low historical difficulties with this cohort in previous years. The service was delivered in two parts in quick succession over two months in November and December 2022. The service delivery involved six pop-up clinics in various public locations around County Durham at weekend followed up with visits to 15 nurseries within the County to provide pre-consented vaccinations.
-
- In total 308 vaccines were administered
-
- ARI Hubs - In January 2023 until March 2023 DDHF, at the request of the ICB extended their Same Day Urgent Care hours in both Bishop Auckland and Durham hubs to provide a service to a specific cohort of adults and children with respiratory symptoms, known as Acute Respiratory Infection (ARI) provided in the same way as the Urgent Care hub with added point of care testing.
-
- In total 856 patients were seen at the ARI hub during this period.
-
- ICB roles - in addition to the above contracts DDHF also recruit and manage, when required, Countywide roles on behalf of the ICB with two of these roles in place at present. Over the past two years we have hosted a Armed Forces Social Prescribing Link Worker part of a 2-year ‘Test and Learn’ Demonstrator funded by NHSE Armed Forces Team to scope out how social prescribing can support the specific needs of the Armed Forces Community (AFC). The funding was due to expire in August 2023 and DDHF have been successful in securing funding for this post for a further year and more details on this can be found in the Services section under Social and Wellbeing Team. Similar to the above role we have also agreed to host an Early Diagnosis Cancer Coordinator to support PCN's and practices throughout County Durham with activities that support early cancer diagnosis for a fixed term of 2 years. This role commenced in April 2023 and more information can be found on this in the Patient Section under Social and Wellbeing Team.
Full CQC inspection was carried out in April 2022 resulting in an overall rating of “Good” with 4 out of 5 key questions within the final inspection report (link this to the CQC report at the bottom of the website) rated as good. The organisation will be focusing on ensuring full assurance is provided as required.
The main current focus for the organisation is to work with the staff, practices, PCN and ICB to retain and sustain the quality of existing services and staff, as well identify opportunities for expansion into new areas and service provision. Working alongside DDHF staff and Additional Role Reimbursement Staff (ARRS) who are a key component of providing the services relating to the Primary Care Network Directed Enhanced Services (PCN DES) contract requirements. Long term the organisation will contribute and collaborate with the PCNs and ICB and Partnership organisations to implement the Integrated Neighborhood Teams in response to the Fuller Report and Recovery of Access to Primary Care guidance issued this year.To be a federation of GP Medical Practices working together to provide high quality cost effective primary healthcare services.
To ensure, maintain and develop the provision of General Practice in the rural and urban communities of Durham Dales.
-
Equity of provision
-
Supportive, caring, and inclusive
-
Performance-oriented
-
Proactive